The Evolving Quadruple Aim and the Importance of Place
Share

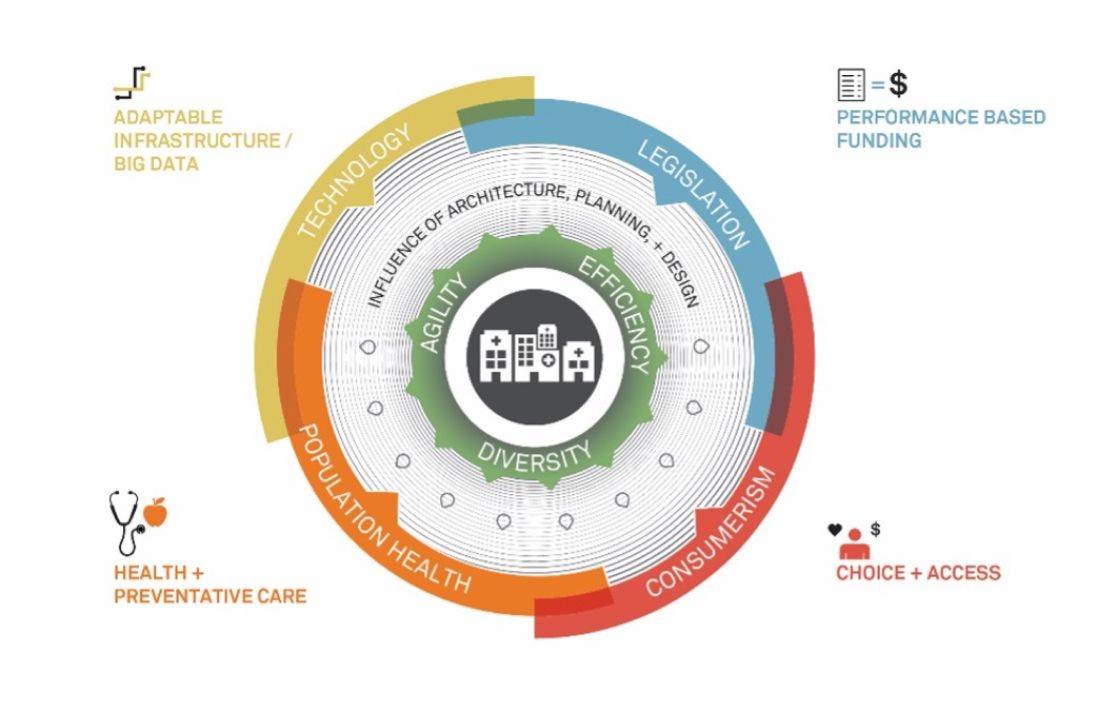
Healthcare networks and their facilities are facing multiple pressures including legislation, population health, the rise of consumerism, and changing technology. These forces press healthcare institutions to adapt to remain competitive and profitable in a value-based system. Healthcare leaders are evaluating new strategies and design models to build a consumer relationship platform with new types of facilities/sites of care and to improve clinical quality and access.
Bending the cost curve of healthcare is a major goal of health networks, consumers, insurers, and legislators alike. In 2009, the Patient Protection and Affordable Care Act (ACA) became law, requiring healthcare networks to adopt pay-for-performance measures, improved patient care, and increased access.
Prior to the ACA, healthcare networks began to optimize overall performance by pursuing each dimension of the Institute for Healthcare Improvement’s (IHI) Triple Aim (2007):
- Improving the health of populations;
- Improving the patient experience of care (including quality and satisfaction); and
- Reducing the per capita cost of health.
Looking forward, The Triple Aim needs to consider the importance of place in creating a continuum of care, as no one size fits all.
When considering the Triple Aim, it is important to acknowledge that patient care outcomes are not always synonymous with patient satisfaction and loyalty. Beyond legislative changes and pay-for-performance measures, patient outcomes and experience should be the focus.
Some may argue that place is covered within the Triple Aim’s dimension of “improving population health,” but with today’s expansive continuum of care — from telemedicine, to outpatient centers, regional hospitals, and major academic medical centers – there is a need to introduce the importance of place as a dimension all its own.

Healthcare networks should broaden strategies from the IHI Triple Aim to The Evolving Quadruple Aim: the right care, at the right time, with the right price, in the right place.
Legislative Changes
The ACA tightened the reins on reimbursements through value-based purchasing, bundled payments, and HCAPHS scores, effectively determining payments. According to the American Journal of Public Health’s January 2016 analysis, 63% of healthcare payments are supported by governmental programs.
The ACA or any new social contract developed by the new administration will continue to impact healthcare delivery, and it is unlikely that reimbursements will rise in the future. Many health networks continue to move forward in a value-based direction and see it as the right way to drive quality and affordability.
Population Health
Population health research attempts to understand the root causes of disease, and ways to mitigate risk factors. According to David Kindig (2014), population health determinants are broken down into four categories:
- Health Behaviors (30%): Includes diet and exercise, along with tobacco and alcohol use
- Clinical Care (20%): Focused on access and quality of care available
- Social & Economic Factors (40%): Includes education, employment, and income
- Physical Environment (10%): The built environment and environmental quality
According to the CDC, chronic diseases are the root cause of two thirds of all deaths and account for three out of every four dollars spent on healthcare. To reduce the cost of chronic care, health networks are developing strategies to increase their access within the communities they serve and effectively meet patients in the exurbs and suburbs.

Penn Medicine Lancaster General Health, Ann B. Barshinger Cancer Institute improves access and management of chronic disease with the goal of providing an extraordinary patient and visitor experience every time.
An architect’s professional responsibility is to protect the health, safety and welfare of the public, and the profession is actively engaged in creating healthier spaces. Evidence based design has now drawn correlations between the built environment and patient outcomes, and design is a catalyst to encourage movement and activity that promotes healthy living.
Rise of Consumerism
Today’s patients have access to information and choice about their care. As high deductible healthcare plans increase, and there is increased transparency in pricing, patients are shopping around for care. When patients shop with their own healthcare dollars, they demand greater value and better experiences.
This rise in consumerism highlights the need for improvement in patient care and experience and the need for facilities which also focus on patient satisfaction. The goal is to improve access to the right facilities in the right place for all patients, while considering consumer preferences.
In order to develop and capitalize on patient loyalty, every visit within the same health system collectively must create a consistently positive experience. Health networks need to build a consumer relationship platform and ensure it translates from facility to facility across the continuum of care.
Changing Technology
Technology is changing faster than ever and its impact on healthcare planning is significant – partly because so much technology is required in healthcare facilities. For example, ACA and MACRA legislation have required significant investment in electronic health records and data management and reporting tools with a direct impact on reimbursements.
With construction budgets constantly under cost pressures, it is important to design spaces with flexibility, targeting those areas, which are most likely to have frequent changes in scope or technology.
It is also important to acknowledge the growing inclusion of big data and its impact on the hospital facilities of tomorrow. As data continues to become more available, how will it be integrated into health networks and facilities to assist patient diagnosis and care planning options in real time?
Technology growth is encouraging the notion of place to expand even further into the community level. As more patients become comfortable with wearable devices, healthcare networks can track patients across more sites of care expanding the continuum of healthcare.
‟Health networks need to build a consumer relationship platform and ensure it translates from facility to facility across the continuum of care.”
Why Place is Crucial to Success: The Evolving Quadruple Aim
The inclusion of place is central to the Triple Aim equation to address population health, improve the patient care quality/experience, and reduce cost.
Awareness of the changes brought by the advent of the ACA and the growth of Internet access is leading to the relocation of many of the services to more convenient and cost-effective venues. When place is taken into account, healthcare networks and planners can “curate” every step of the patient interaction, an interaction that begins even before leaving home.
Lower acuity care remains close to the patients at home, follow up and primary care is accessible “on demand”, and it is only when patients are facing more acute or complicated care that they travel to the higher acuity care options. With various locations for patients to receive the level of care they need — close to home and at a variety of price points — a health network can behave as an organism coordinating all its parts.
Future success will require a different playbook than the one health systems are operating with today and must react to the growing demand for patients to receive great care when they need it, where they need it, for a price they can afford.
The initial 2015 and 2016 Site Neutrality Rulings from the Centers for Medicare and Medicaid Services (CMS) limit any outpatient facility from maintaining the technical fees and hospital-based pricing if they are opened more than 250 yards from a hospital. These rulings appear to run counter to the goal for care closer to patients in their communities. While attempting to provide more low-cost options for patients closer to home, this ruling may create barriers for future construction of care centers within the community.
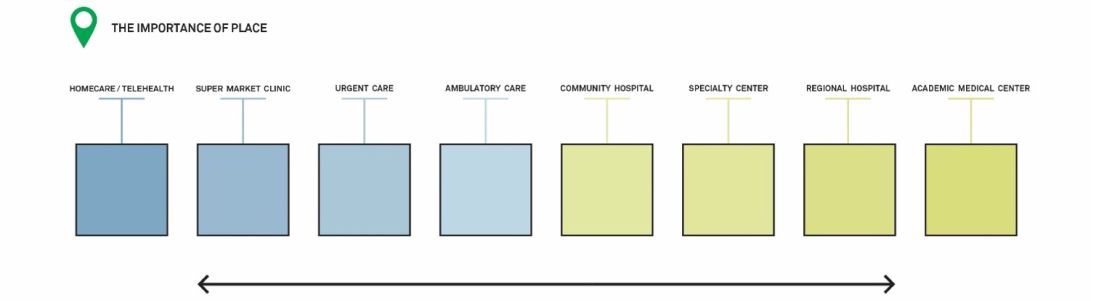
Example of the continuum of care : A consumer relationship platform to build patient loyalty
Navigating today’s healthcare landscape, health networks and architects must act together with agility and efficiency to put forth a diversity of healthcare facility solutions — collaborating to bend the cost curve by designing for the entire continuum of facilities that deliver the right care, at the right time, with the right price, in the right place.

The HealthPlex for Advanced Surgical and Patient Care is committed to advancing health and transforming lives. This regional hospital is home to an 88,000 SF green roof that provides access to patients, families, staff and the community.